If you’re frequently tired, chilled, forgetful, or irritable despite sleeping and exercising, low intake could be the cause. These symptoms often reflect inadequate calories, carbs, or protein and can affect hormones, mood, and digestion. This is practical, evidence‑based stuff — keep going to see specific signs and clear steps you can take.
Persistent Fatigue and Low Energy

When you consistently eat less than your body needs, your cells run short on the fuel they need to make energy, and you’ll notice persistent tiredness, difficulty concentrating, lightheadedness, and poor exercise tolerance. You can test this: track intake and energy across a week, noting sleep, activity, and timing. Low caloric or carbohydrate intake reduces glycogen and ATP production, impairing cognitive focus and endurance. Prioritize small, nutrient-dense meals and strategic snacks—protein with complex carbs and a bit of healthy fat—to stabilize blood glucose and restore performance. Consider targeted adjustments (calories, meal frequency, macronutrient balance) and monitor responses objectively. If fatigue persists despite thoughtful refeeding and sleep hygiene, seek metabolic or medical evaluation. This pragmatic, data-driven approach helps you regain sustainable energy and function again.
Irritability, Anxiety, or Mood Swings

If you’re not eating enough, drops in blood sugar can make you irritable, shaky, and lightheaded. Low glucose also triggers stress hormones that can heighten anxiety and cause sudden mood swings. Noticing these changes? Try regular small meals with carbohydrate plus protein and check in with a clinician if anxiety or mood shifts persist.
Low Blood Sugar Effects
Because your brain depends on a steady glucose supply, even modest drops in blood sugar can trigger sudden irritability, anxiety, or mood swings that you’ll notice as sharp shifts in emotion or concentration. You may feel jittery, lightheaded, or irritable; these are typical signs of glucose deficit. Practical steps work: schedule regular meals, pair protein and fiber with carbs, and carry snacks like nuts or fruit. Log timing of symptoms to refine meals and portions. If you use glucose lowering medication or have diabetes, monitor levels and coordinate adjustments with your clinician. If mood shifts remain frequent or strong despite these strategies, seek evaluation to rule out metabolic or medical causes. These evidence informed approaches help you stabilize energy and reduce sudden emotional swings.
Anxiety and Mood Changes
Although it’s easy to blame stress, inadequate calorie intake can rapidly alter your brain chemistry and trigger irritability, anxiety, or sudden mood swings. When you don’t eat enough, neurotransmitter production—serotonin, dopamine—drops, and cortisol rises, which research links to heightened anxiety and emotional lability. You may notice decreased tolerance, snap judgments, or persistent low mood that improve after eating. Practical steps: track intake for a few days, prioritize balanced meals with protein and healthy fats, schedule small regular snacks, and test changes before altering routines. If mood instability persists despite refueling, consult a clinician; mood shifts can reflect other conditions. This client-centered, evidence-based approach helps you prototype sustainable eating patterns that stabilize mood and boost cognitive resilience. You’ll feel more grounded as intake normalizes consistently.
Trouble Concentrating or Brain Fog
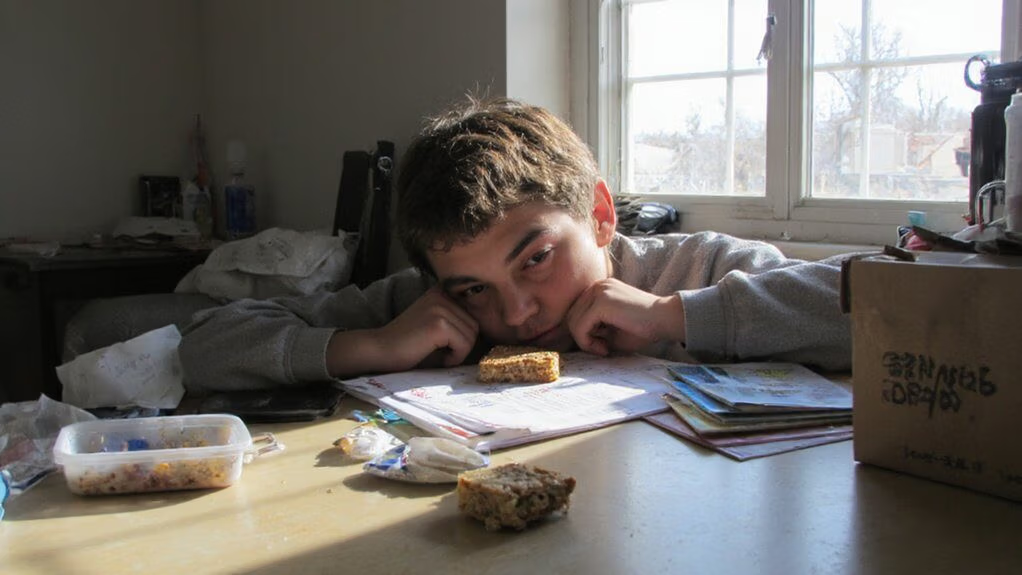
When you consistently eat too little, your brain quickly shows it as trouble concentrating or a persistent “brain fog.” Low calorie intake reduces blood glucose and limits the raw materials for neurotransmitters (like serotonin and dopamine), while chronic deficits in iron, B12, vitamin D and other nutrients further impair cognitive speed and memory. You’ll notice slowed thinking, fuzzy recall, and difficulty completing complex tasks. Start with targeted, practical steps to restore cognition: prioritize balanced meals, include protein and healthy fats, and monitor nutrient status. Actions:
- Reintroduce regular meals with 300–500 kcal snacks combining carbs and protein.
- Test iron, B12, vitamin D and act on deficits with clinician guidance.
- Simplify tasks, use timers, and stagger demanding work while you recover.
Small, measurable changes restore clarity.
Frequent Lightheadedness or Dizziness
You might feel lightheaded or dizzy when you haven’t eaten enough — that’s often due to low blood sugar episodes that briefly reduce the fuel your brain needs. Standing up quickly can trigger postural dizziness because low energy and reduced blood volume make it harder to maintain blood pressure. Also consider dehydration and electrolyte loss, which commonly accompany poor intake and can worsen symptoms; try regular small meals or snacks, adequate fluids, and an oral electrolyte option if your clinician agrees.
Low Blood Sugar Episodes
Ever feel sudden lightheadedness, sweating, or shaky weakness between meals? Those are classic hypoglycemia signals when you haven’t replenished glucose. You can act fast to stabilize symptoms and prevent episodes. Prioritize small, balanced snacks, monitor patterns, and consult if events recur.
- Keep a portable 15 to 20 g quick-carb option (juice, glucose gel) for immediate response.
- Pair future meals with protein and healthy fats to slow glucose drops and sustain energy.
- Track timing, triggers, and severity to guide adjustments or professional evaluation.
This approach is evidence-informed, practical, and client-centered, giving you simple, innovative strategies to reduce low blood sugar episodes and regain confidence in daily energy management. If you’re diabetic, coordinate changes with your healthcare team promptly for safety.
Postural Dizziness on Standing
Although standing up quickly can trigger a sudden drop in blood pressure (orthostatic hypotension) and cause lightheadedness, frequent episodes often reflect low fluid or salt intake, prolonged fasting, certain medications, or autonomic changes—so you’ll want to address intake and medication factors first. If you notice repeated lightheadedness, track timing relative to meals, medication times, and activity. Check supine-to-standing blood pressure and heart rate with your clinician to distinguish volume issues from autonomic dysfunction. Try pragmatic steps: rise slowly, sit if dizzy, eat small regular protein-and-fat containing snacks to stabilize energy, and avoid long fasts. Review prescriptions and over-the-counter drugs with a provider; dose adjustments or alternatives can reduce symptoms. Consider compression garments and structured reconditioning if autonomic causes are suspected. Act promptly for improvement.
Dehydration and Electrolyte Loss
When you’ve been losing more fluids or salts than you take in—through sweating, diarrhea, vomiting, fever, or diuretic use—you’ll often feel lightheaded or dizzy because blood volume and electrolyte balance drop and impair circulation and brain perfusion. You should recognize this as a physiological signal that your intake is inadequate or imbalanced. Rehydrate with targeted fluids and electrolytes, not just water, and prioritize small frequent meals that include sodium, potassium and magnesium. Track urine color and weight; consider point-of-care electrolyte testing if symptoms persist. Try oral rehydration solutions or low-sugar electrolyte mixes. Get medical review for severe or recurrent dizziness to exclude cardiac or neurologic causes promptly.
- Check urine color and output
- Replace sodium, potassium, magnesium
- Seek testing for persistent symptoms
Feeling Unusually Cold or Chilled
If you’re feeling unusually cold or chilled despite wearing enough layers, it may be a sign you’re not eating enough; low calorie intake lowers your resting metabolic rate and reduces heat production, and over time loss of body fat and muscle can diminish insulation and warmth. You should track patterns: note when chills occur relative to meals, activity, and sleep. Consider modestly increasing calorie intake with nutrient-dense options—protein, healthy fats, and caloric carbohydrates—to support thermogenesis and preserve lean mass. Monitor resting heart rate, energy, and subjective warmth as objective markers of recovery. If adjustments don’t help within a couple weeks or you feel faint, consult a clinician for metabolic, thyroid, or anemia evaluation. Small, iterative changes reduce risk and support sustainable adaptation and resilience.
Hair Thinning, Brittle Nails, or Dry Skin
Because your body redirects nutrients to essential organs, inadequate calorie and protein intake often shows up in hair thinning, brittle nails, or dry skin — signs that keratin and lipid synthesis are impaired. You may notice slower hair growth, increased shedding, split ends, dull nails that peel, or flaky, rough skin. These are clinical clues that protein, essential fatty acids, zinc, iron, and biotin are insufficient. Practical steps include reviewing intake, prioritizing nutrient-dense foods, and measuring objective markers with your clinician. Try innovations: reframe meals for protein at each eating occasion and add plant and marine omega sources. Monitor progress over weeks, not days. Adjustments should be individualized and data-driven. Stay curious.
- Track protein per meal
- Add omega-rich foods
- Check labs with a provider
Digestive Problems and Constipation
Low calorie and low-fiber eating patterns often slow gut motility, so you may notice fewer bowel movements, hard or pellet-like stools, straining, or bloating alongside the other signs of undernutrition. If you’re experiencing constipation, reassess energy intake, fiber diversity, hydration, and meal timing—each influences transit time. Aim to incrementally increase whole-food fiber (fruits, vegetables, legumes, intact grains) and distribute intake across the day to support microbiome activity. Prioritize consistent fluids and consider tolerance-based increases in soluble and insoluble fiber rather than abrupt changes that cause gas. When appropriate, integrate gentle physical activity to stimulate motility. Track patterns to identify triggers and collaborate with a clinician before using laxatives or supplements. Small, measurable adjustments often restore regularity while preserving your broader recovery goals and resilience.
Irregular or Missed Menstrual Cycles
If you’re under-eating, your body may stop ovulating and develop hypothalamic amenorrhea, which shows up as irregular or missed periods. Low estrogen from energy deficiency raises your risk of bone loss, fatigue, and mood changes. If your cycles change or stop, talk with a clinician to assess your energy intake and plan recovery steps.
Hypothalamic Amenorrhea
When you start missing periods or your cycle becomes irregular, it can signal hypothalamic amenorrhea—a condition where inadequate energy intake or excessive exercise suppresses the brain’s release of GnRH, lowering LH/FSH and estrogen and stopping ovulation. You need an evidence-based, individualized plan: restore energy availability, reduce excessive training, and reassess stress and sleep. Track patterns objectively, work with a clinician or dietitian who understands relative energy deficiency, and set measurable recovery goals. Early intervention often reverses dysfunction without invasive measures. Consider these core actions:
- Prioritize consistent caloric intake matched to activity.
- Scale back high-volume/intensity exercise temporarily.
- Optimize sleep and stress management alongside nutrition.
You’ll regain cycles by restoring balance and monitoring progress clinically. Measure hormones and symptoms periodically with professional guidance and patience.
Low Estrogen Consequences
Because estrogen plays a central role in reproductive, bone, cardiovascular, and metabolic health, losing regular periods can quickly affect more than just fertility: you may notice hot flashes, vaginal dryness, low libido, mood changes, and increasing fracture risk from accelerated bone loss, and over time your cardiovascular profile can worsen. Low estrogen from undernutrition suppresses ovulation; your cycle becomes irregular or stops. This isn’t just reversible by willpower—restoring energy availability and reducing stressors usually returns menses and restores bone turnover, but delayed recovery raises long-term osteoporosis and heart disease risk. Work with clinicians to measure hormones, bone density, and tailor nutrition, sleep, and training plans. Prioritize progressive energy refeeding and monitored exercise adjustments so you regain hormonal balance and protect long-term health and resilience.
Loss of Muscle Mass and Physical Weakness
Even with regular activity, you may notice clothes becoming looser around your arms and legs and tasks like carrying groceries or climbing stairs feeling harder than they used to. Losing lean mass when calorie intake’s too low reduces strength, metabolic rate, and functional capacity. Assessments like grip strength or simple chair-stand tests help quantify change and guide choices. Prioritize progressive resistance, adequate protein (0.8–1.2 g/kg or individualized), and strategic calorie repletion under clinician guidance to rebuild muscle.
- Track objective metrics (strength, body composition, performance)
- Adjust nutrition with targeted protein and energy increases
- Use structured resistance programs and monitor recovery
You deserve practical, measurable steps—apply them iteratively and consult a professional to personalize the plan. Expect gradual improvements; track data and adapt based on outcomes.
Sleep Disturbances and Trouble Falling Asleep
Low calorie intake can disrupt your sleep, making it harder to fall asleep and stay asleep. When you chronically underfuel, your body raises cortisol and lowers leptin and thyroid hormones, which can fragment sleep cycles and reduce REM and deep sleep. You may notice midnight awakenings, early-morning wakefulness, or daytime sleepiness despite time in bed. Addressing this is practical: restore consistent, adequate calories, include evening protein and complex carbs to stabilize glucose, and time meals to support circadian rhythms. Track sleep and intake for two weeks to spot patterns; consider working with a dietitian or sleep specialist to adjust intake without overshooting goals. Small, measurable changes often yield rapid improvements in sleep quality and daytime function and reduce anxiety linked to inadequate nutrition rapidly.
Conclusion
If you’re noticing persistent fatigue, cold sensitivity, mood changes, brain fog, dizziness, digestive issues, missed periods, or muscle loss, you’re likely under‑fueling. Track your intake, sleep and symptoms, and prioritize regular nutrient‑dense meals with protein, carbohydrates and healthy fats. Make gradual, sustainable changes and monitor how you feel. If symptoms persist, you should see a healthcare provider for evaluation and labs to rule out medical causes and guide a safe, individualized plan and recovery timeline.