You often won’t feel high blood pressure, yet certain signs merit attention: persistent bilateral throbbing morning headache, visual disturbances, chest pain or dyspnea, reduced urine output, or sudden neurological deficits. These findings suggest end‑organ strain or hypertensive emergency and demand prompt evaluation; knowing their typical patterns and thresholds for action can substantially alter outcomes—here’s what to watch for next.
What High Blood Pressure Means for Your Health

If you have high blood pressure, sustained elevations in arterial pressure increase shear stress and promote endothelial dysfunction, accelerating atherosclerosis and raising your risk of myocardial infarction, stroke, heart failure, and chronic kidney disease. You should understand that hypertension drives target-organ damage via mechanotransduction, oxidative stress, inflammation, and maladaptive remodeling; ambulatory blood pressure, pulse wave velocity, and central aortic pressure provide superior prognostic information compared with office readings. You’ll benefit from integrated risk assessment combining home monitoring, biomarkers (hs-CRP, NT-proBNP, urine albumin-creatinine ratio), and imaging (carotid ultrasound, echocardiography) to guide therapy intensity. Contemporary management leverages individualized pharmacotherapy, device-based modalities, and digital therapeutics to optimize control and reduce cardiovascular event rates, aligning care with precision-medicine principles. You’ll also prioritize longitudinal data integration to refine outcomes.
Common Physical Symptoms to Watch for
You should monitor for frequent headaches, since epidemiological and clinical data link recurrent cephalalgia with uncontrolled hypertension and hypertensive crises. You may notice blurred or reduced vision from hypertensive retinopathy or acute ischemic events affecting ocular perfusion. You might develop shortness of breath from hypertensive heart disease, pulmonary edema, or comorbid cardiopulmonary pathology, and these signs warrant prompt clinical evaluation.
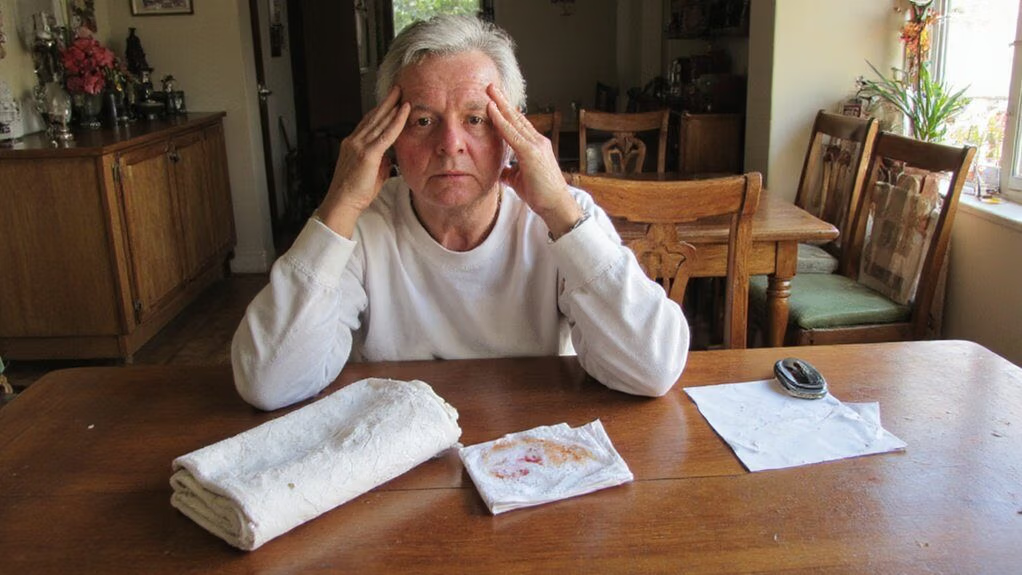
Frequent Headaches
Frequently, patients with uncontrolled or severely elevated blood pressure report persistent, often bilateral headaches that are throbbing and worst on awakening. You should recognize these cephalalgias as potential hypertensive manifestations mediated by increased intracranial arterial pressure, endothelial dysfunction, and neurogenic inflammation. Measure ambulatory and office pressures to correlate symptom temporality; single readings aren’t diagnostic. You’ll integrate headache phenotype, blood pressure variability, and response to antihypertensive initiation when stratifying risk for hypertensive emergency. Neuroimaging is indicated if focal deficits, altered mental status, or atypical features appear. Use validated headache scales and continuous BP monitoring in research-grade assessments to quantify burden and treatment effect. Early, protocolized titration of antihypertensive therapy reduces cerebral autoregulatory strain and symptom persistence, aligning with precision-medicine goals and improves long-term cardiovascular outcomes.
Blurred or Reduced Vision
When acute or sustained hypertension injures ocular structures, you may experience blurred or reduced vision from hypertensive retinopathy, optic nerve ischemia, or occipital‑lobe dysfunction. You’ll note transient visual obscurations, scotomas, metamorphopsia, or progressive visual-field constriction correlating with arteriolar narrowing, cotton‑wool spots, retinal hemorrhages, and macular edema on fundoscopic exam. High intraluminal pressure compromises autoregulation, producing ischemic neuronal injury detectable by OCT, fluorescein angiography, or visual-evoked potentials. Rapid BP reduction or malignant hypertension can precipitate acute vision loss; conversely, chronic poorly controlled hypertension yields gradual decline. Management requires prompt blood-pressure normalization, targeted neuro-ophthalmologic assessment, and advanced imaging to stratify risk and monitor recovery. You should pursue interdisciplinary care integrating hypertension control, ocular intervention, and functional testing to preserve vision and guide innovation in therapeutic strategies.
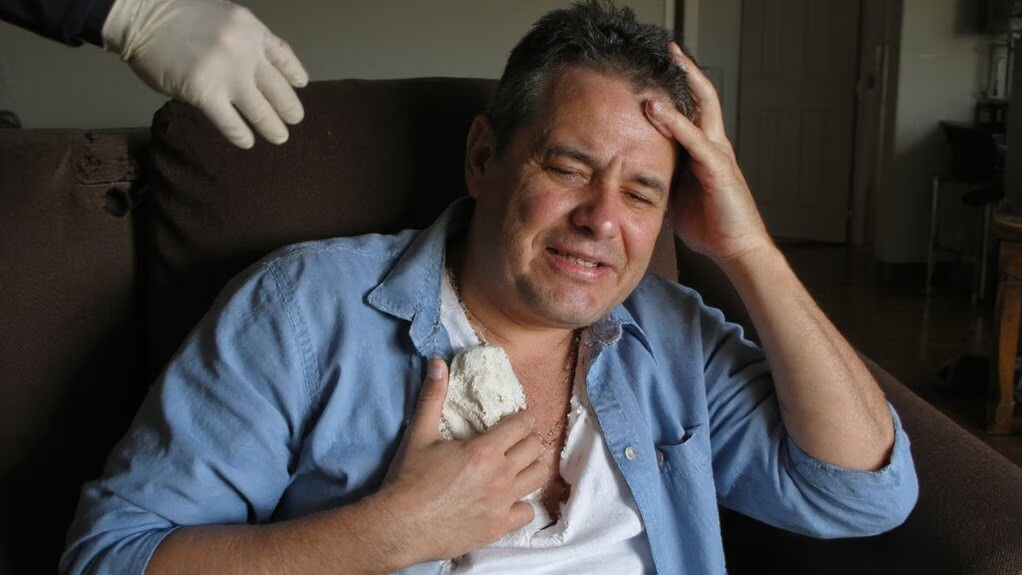
Shortness of Breath
If sustained or acute elevations in blood pressure occur, they can produce shortness of breath through multiple cardiopulmonary mechanisms. You may experience exertional dyspnea, orthopnea, or paroxysmal nocturnal dyspnea as hypertension increases left ventricular afterload, promotes concentric hypertrophy, and precipitates diastolic dysfunction. Elevated systemic pressures raise pulmonary venous pressure, cause interstitial pulmonary edema, and reduce pulmonary compliance, which limits gas exchange and increases ventilatory demand. You should monitor symptoms alongside objective metrics: resting respiratory rate, pulse oximetry, BNP, echocardiographic diastolic indices, and ambulatory blood pressure. Rapid onset dyspnea with hypoxia warrants emergent evaluation for hypertensive heart failure or pulmonary edema. You should engage multidisciplinary teams for personalized, technology-enabled care delivery.
Sudden Severe Spikes and Emergency Signs
Because blood pressure can rise abruptly, clinicians distinguish a hypertensive emergency—generally systolic ≥180 mm Hg or diastolic ≥120 mm Hg accompanied by acute target‑organ injury—from hypertensive urgency, which lacks evidence of end‑organ damage. You must recognize rapid deterioration: symptoms indicate end‑organ ischemia or failure and require immediate evaluation and controlled blood‑pressure reduction in monitored settings. Watch for:
- Sudden severe headache with altered consciousness suggesting hypertensive encephalopathy or intracranial hemorrhage.
- New focal neurological deficits indicating possible stroke.
- Acute visual loss or papilledema from malignant hypertensive retinopathy.
- Oliguria or rising serum creatinine signaling acute hypertensive nephropathy.
- Seizures as a manifestation of cerebral hyperperfusion or hemorrhagic complication.
Act promptly; delayed intervention increases morbidity. You should activate emergency services and reach a monitored facility offering parenteral antihypertensive therapy.
How High Blood Pressure Affects Your Heart and Vessels
After acute hypertensive events, you should recognize that sustained elevation of arterial pressure imposes chronic hemodynamic load and biologic injury on the heart and vasculature. You’ll develop concentric left ventricular hypertrophy as myocytes adapt to increased afterload, which raises myocardial oxygen demand and predisposes you to ischemia. Hypertension accelerates endothelial dysfunction, promotes inflammation, and markedly enhances atherogenesis in medium and large arteries. Increased arterial stiffness raises pulse pressure and transmits pulsatile stress to microcirculation, causing rarefaction and remodeling. Persistent pressure overload impairs diastolic relaxation and can progress to heart failure with preserved ejection fraction. Vascular remodeling and plaque rupture increase your risk of coronary events. Hypertensive remodeling fosters arrhythmogenic substrates via fibrosis and altered conduction. Targeted hemodynamic control and novel therapies can limit changes.
Vision Changes and Neurological Warning Signs
When blood pressure rises acutely or remains uncontrolled, you’ll often see direct effects on the visual apparatus and central nervous system that signal end-organ injury. You may notice transient visual obscurations, visual field deficits, or sudden painless vision loss from hypertensive retinopathy, retinal artery occlusion, or optic neuropathy. Neurological warning signs include focal weakness, aphasia, acute severe headache, altered consciousness, and seizure—these reflect hypertensive encephalopathy, intracerebral hemorrhage, or ischemia. Rapid recognition and emergent imaging guide intervention. Monitor neurologic status, visual acuity, funduscopy, and blood pressure trends; escalate to stroke or neuro-ophthalmology services when indicated. Key clinical features to watch for:
- Sudden monocular or binocular vision loss
- Visual field cuts or scotomas
- Papilledema on funduscopy
- Focal neurologic deficits
- Hypertensive headache
When Lifestyle and Stress Contribute to Hypertension
Although individual susceptibility varies, modifiable lifestyle behaviors and psychosocial stressors substantially increase both the incidence and severity of hypertension. You should recognize that sustained sympathetic activation, poor diet, sedentary behavior, sleep disruption and excess alcohol potentiate vascular resistance and dysregulate neuroendocrine control. Interventions targeting these domains demonstrably reduce ambulatory pressures and end-organ risk when implemented early. Use metrics and iterative feedback to optimize adherence and physiologic response.
| Factor | Mechanism |
|---|---|
| High sodium intake | Increases plasma volume, raises cardiac output |
| Chronic stress | Activates HPA axis, elevates catecholamines |
You must integrate behavioral modification with precision therapeutics and scalable monitoring to innovate care pathways. Measure outcomes with reproducible biomarkers and AI-enabled analytics to refine individualized treatment algorithms rapidly. You’ll prioritize risk stratification and implementation science throughout. Immediately deploy.
How to Monitor Blood Pressure at Home
You should select an automated oscillometric upper‑arm monitor that’s been validated against clinical standards and paired with a cuff sized to your mid‑upper arm circumference. Check validation listings and choose a model that records multiple readings and reports averages to improve reliability. When you measure, sit quietly and place the cuff on the bare upper arm at heart level with the bladder centered over the brachial artery, fitting it snugly but not tightly.
Choosing a Home Monitor
How do you select a device that will give clinically reliable readings? You prioritize validated, automated oscillometric monitors with documented accuracy in peer-reviewed protocols. Choose upper-arm devices over wrist models unless validation data supports wrist use. Prefer units with memory, averaging algorithms, and calibrated pressure sensors. Integrate connectivity (Bluetooth/USB) for secure data export to clinicians and analytic platforms. Confirm independent validation by organizations such as dabl, ESH, or AAMI.
- Device validated against clinical protocols
- Upper-arm oscillometric mechanism
- Digital averaging and artifact rejection
- Secure connectivity and data export
- Clear maintenance/calibration pathway
You’ll verify cuff size compatibility but will address placement separately; focus here remains device performance and interoperability. Also review long-term battery stability, firmware update policy, and institutional support for device integration into health systems.
Proper Cuff Placement
Because proper cuff placement directly affects measurement accuracy, place the cuff on the bare upper arm with the bladder centered over the brachial artery, about 2–3 cm proximal to the antecubital fossa. You should align the cuff marker with the artery, maintain snug but not compressive fit (one finger under edge), and position your arm supported at heart level to minimize hydrostatic bias. Use manufacturer-recommended cuff size; using an incorrect circumference yields systematic error. If you have atrial fibrillation or vascular pathology, repeat measurements and average per guidelines. For innovation-minded users, consider cuff-integrated sensors and automated positional feedback available in advanced monitors to verify alignment and detect movement artifacts. Document cuff size, arm used, posture, and time for reproducible home monitoring and clinical correlation.
When to Seek Medical Attention
When should you seek immediate medical attention for high blood pressure? You should act if readings or symptoms suggest hypertensive emergency or acute end-organ dysfunction; rapid evaluation reduces morbidity. Seek care when you observe:
- Systolic ≥180 mmHg or diastolic ≥120 mmHg with signs of organ damage
- Chest pain, acute coronary syndrome features, or ischemic symptoms
- Neurological deficits, severe headache, confusion, vision changes, or stroke signs
- Shortness of breath, pulmonary edema indicators, or acute heart failure symptoms
- Severe renal impairment, oliguria, or rapidly rising creatinine
Inform clinicians about home-monitoring trends, medication adherence, and recent interventions. Expect protocolized triage, rapid diagnostics, and guideline-driven medication titration for outcomes.
Conclusion
You should recognize that hypertension is frequently asymptomatic, yet persistent bilateral throbbing morning headaches, acute severe headache with neurologic deficits, visual disturbances, chest pain, dyspnea, oliguria, or edema signal end‑organ strain and require prompt evaluation. You’ll monitor at home with validated devices, document readings, and adjust lifestyle and medications per guideline targets. If readings remain severely elevated or symptoms occur, you must seek immediate medical care to reduce morbidity and mortality and prevent organ complications.