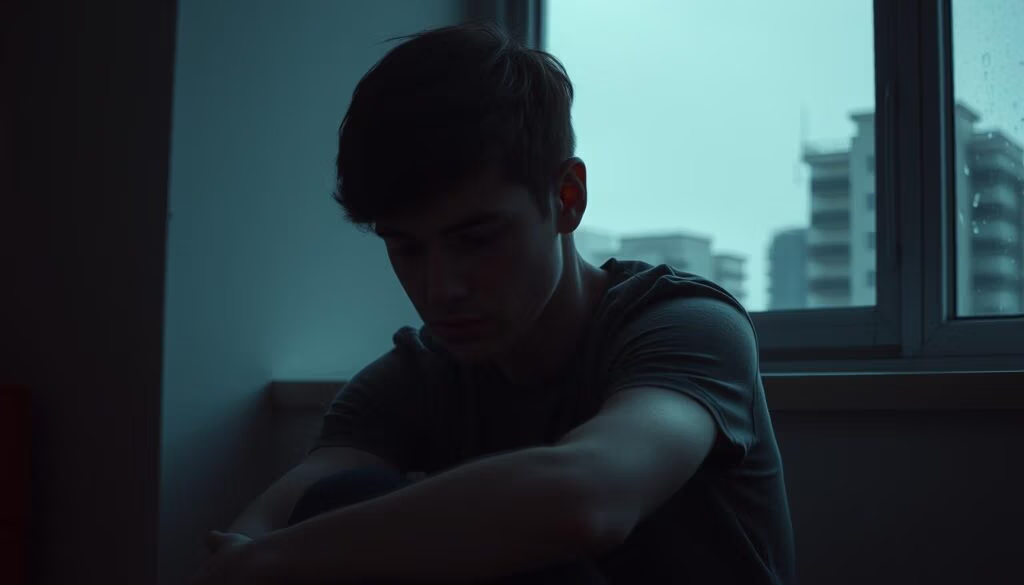
You may look steady and able at work, home, or in public, yet feel weary inside. High-functioning depression describes when depressive symptoms quietly sap your energy while you still meet daily demands. This can make your inner life feel heavy even as others see no change.
You might notice low mood, less joy, trouble focusing, sleep shifts, or negative self-talk. These symptoms mirror major depression but can hide behind steady productivity. That mismatch—what you show versus what you feel—takes a real toll.
The effort you spend to keep going can be far greater than it seems. Causes vary from genes to stress, and masking makes it easy for loved ones or coworkers to miss what’s happening. You deserve care that restores your energy and quality life, not just a way to keep doing things.
Key Takeaways
- You can appear fine while feeling persistently low inside.
- Symptoms overlap with major depression even when you keep functioning.
- The hidden effort to cope can wear you down over time.
- Causes include genetics, hormones, and stress; masking hides the need for help.
- Treatment can improve your mood, energy, and overall quality of life.
High-Functioning Depression Explained: What It Is—and What It Isn’t
You may keep up routines and still carry a constant, draining inner weight. This phrase describes people who meet daily roles while feeling low inside. It is not a formal DSM-5 diagnosis, but it names a real mental health experience many live with.
How it looks: by day you can appear productive and engaged. You use masking and compensation to get through the workday, then feel wiped out at home or disconnected on social platforms.
Where it fits with other disorders
High-functioning depression may overlap with persistent depressive disorder (PDD or dysthymia), which is milder but long-lasting. It can also sit near clinical depression, though major depressive disorder more often causes clear impairment in functioning.
Because performance metrics stay decent, friends and clinicians can miss this hidden dysfunction. Still, chronic low-grade symptoms are an illness worth care. Early therapy or treatment can shorten the time you struggle and help you protect your energy and life satisfaction.
- Not a formal label, but a helpful way to explain persistent symptoms.
- Masking can hide serious need for support.
- Using accurate terms like PDD or depressive disorder helps when you seek assessment and therapy.
Signs of High-Functioning Depression
You keep showing up, while a steady, low hum of fatigue and doubt follows you through the day.
Subtle daily symptoms you might dismiss
Low mood that lasts most days can feel like normal stress. Joy arrives briefly and then fades. Simple tasks take extra effort, and you may tell yourself it’s temporary.
Body and behavior changes
Sleep or appetite shifts, weight change, and trouble concentrating are common. Energy stays low despite adequate rest. These physical symptoms mirror broader depressive symptoms and matter for your care.
Emotional patterns and the hidden cost
Hopelessness, guilt, harsh self-talk, and irritability can dominate your inner life. You may function at work or home but feel drained after social activities or parenting. That functioning has a real cost.
Children and teens
Young people may mask sadness while keeping grades. Watch for isolation, increased screen time, sleep or appetite changes, self-injury, or talk of suicide. If there’s imminent danger, call 911; for confidential support, call or text 988.
| Area | Common symptoms | What to watch for |
|---|---|---|
| Mood | Persistent low mood, brief joy | Feeling flat most days |
| Body | Sleep, appetite, weight changes | Fatigue despite rest |
| Function | Keeps working but with cost | Draining social activities |
| Youth | Masking, school strain | Isolation, increased screen time |
High-Functioning vs. Major Depression vs. PDD: How They Differ
Understanding whether symptoms disrupt daily roles or quietly sap your energy is key to finding the right help.
Severity: Major depression often brings intense symptoms that impair work, school, or home life. In contrast, high-functioning depression can have similar symptoms but with preserved external performance and a high internal cost.
Duration: Persistent depressive disorder (PDD) involves a chronic, low mood that lasts for years. Major depression tends to come in distinct episodes. High functioning patterns can appear in either setting.
Functioning, masking, and hidden dysfunction
If you keep meeting obligations but it feels unsustainably hard, you are in the high functioning zone. You may excel at work while neglecting chores, relationships, or self-care.
Masking—selective posting, steady output at the office, or private weekend crashes—creates an illusion that everything is fine.
“People often miss the real impact because they judge by what they see, not by how you feel.”
- Anhedonia, fatigue, sleep and appetite shifts, concentration trouble, and irritability can occur across all three conditions.
- The difference lies in intensity and how much these symptoms limit daily roles.
- Clarify whether you’re facing a chronic depressive disorder, a discrete clinical depression episode, or both when you talk with a provider.
| Feature | Major depression | PDD | High functioning |
|---|---|---|---|
| Severity | High, often disabling | Milder, long-term | Moderate intensity, hidden cost |
| Duration | Episodic | Years | Can be episodic or chronic |
| Functioning | Often impaired | Variable | External performance preserved |

Why this matters: Accurate language guides treatment, follow-up, and your path to better mental health. Track frequency and impact of symptoms across weeks and share that record with your clinician to shape care that protects your life and recovery.
Treatment and Daily Coping: How You Can Feel Better Starting Today
You can start changing how you feel today by combining therapy, habit shifts, and practical supports.
Therapy matters. Cognitive behavioral therapy (CBT) teaches you to challenge negative thoughts and rebuild routines that lift mood and functioning. For teens, interpersonal therapy (IPT-A) focuses on relationships and communication. Parent-management approaches help caregivers shape healthy behavior when kids struggle.
When medication helps
Medication like SSRIs can ease persistent low mood, sleep disruption, and concentration problems. Research shows combined therapy and medication often works best for young people with major depression. Your clinician can tailor a plan to your needs.
Daily habits that support recovery
Small, consistent actions change your day. Aim for steady sleep, short outdoor walks, nourishing meals, and scheduled breaks. Limit social screen time that fuels comparison and isolation.
“Early treatment protects your quality life and the energy you need to keep functioning.”
- Build micro-wins: ten-minute tasks and light movement.
- Create a simple tracker for sleep, energy, appetite/weight, and mood.
- Keep a support network: a therapist, primary care clinician, and one trusted person.
If you want detailed guidance on care and treatment options, see depression treatment recommendations. Acting now gives you a better chance to protect your life and regain steady energy.
Conclusion
Even when tasks get done, the inner toll can build quietly over weeks and months. If you suspect high-functioning depression, remember that this mental health condition is common and treatable. You don’t have to keep carrying the burden alone.
Use the signs and symptoms outlined here to start a simple conversation with a provider. Ask whether your pattern fits PDD or a clinical depression episode so your treatment matches your needs.
Start one small thing today: schedule an appointment, try a mood tracker, or tell a trusted loved one what you’re facing. These actions shift hidden effort into shared support and real change.
If you feel at risk now, call or text 988; for immediate danger, call 911.
FAQ
What does it mean when you feel low but still handle work and family?
You may be experiencing a persistent low mood that doesn’t stop you from meeting obligations but does reduce your joy and energy. This pattern can mirror persistent depressive disorder (PDD) or a milder depressive condition where you keep functioning outwardly while struggling internally. Talk to a clinician if fatigue, negative self-talk, or loss of interest lasts for weeks.
How can this condition look “fine” to others while you feel awful inside?
People often mask symptoms by keeping routines, meeting deadlines, and socializing. Masking hides sleep changes, concentration problems, or irritability you battle daily. Because you meet expectations, friends and coworkers may not notice your distress — but that doesn’t make the experience any less real or damaging to your health.
What typical daily signs should you stop dismissing as just a “rough patch”?
Pay attention to persistent low mood, reduced pleasure in activities, needing more effort to get through tasks, and increasing negative self-talk. Changes in sleep, appetite, energy, or concentration that last weeks are important. If these affect your quality of life or cause mounting guilt and hopelessness, reach out for support.
How do sleep, weight, and concentration changes relate to this condition?
Disrupted sleep, unexplained weight shifts, and trouble focusing are common physical and cognitive signals that your mood is affecting brain and body function. These symptoms often worsen fatigue and make daily tasks feel heavier. Tracking patterns can help clinicians recommend targeted strategies like behavioral activation or medication when appropriate.
Can children and teens show different warning signs than adults?
Yes. Young people may mask distress, fall behind at school, withdraw from activities, increase screen time, or show self-harm behaviors. Irritability and academic or behavioral changes can be key red flags. Early intervention with family-based strategies and evidence-based therapies improves outcomes.
How do you tell the difference between this pattern and major depression or PDD?
Duration and severity matter. Major depression often causes marked impairment and distinct episodes, while PDD involves a longer-lasting, lower-grade depressive state. The “functioning” aspect means you might still meet roles despite suffering. A mental health professional can assess severity, duration, and impact to guide diagnosis and treatment.
What treatment options actually help you feel better?
Evidence-based psychotherapy such as cognitive behavioral therapy (CBT) or interpersonal therapy (IPT) can reduce symptoms. For some people, selective serotonin reuptake inhibitors (SSRIs) or combined care (therapy plus medication) are effective. Tailored plans, routine follow-up, and lifestyle adjustments improve results.
What everyday habits can support your recovery starting now?
Prioritize regular sleep, balanced nutrition, gentle physical activity, and small, consistent social contact. Structure your day with achievable tasks and use stress-relief practices like deep breathing or brief walks. These steps won’t replace therapy but can reduce symptom severity and boost resilience.
When should you seek professional help immediately?
Contact a clinician now if you experience worsening hopelessness, suicidal thoughts, significant sleep or appetite disruption, or marked decline in functioning. If you’re unsure, reach out to your primary care doctor, a mental health provider, or a crisis line for expedited support.
How can loved ones best support you if they suspect you’re struggling?
Encourage open conversation without judgment, offer help finding professional care, and assist with practical tasks when you feel overwhelmed. Validating your experience and helping you connect with therapy or medical evaluation can make a major difference in your recovery.